May 30, 2025
Signs of Ovulation: How to Track and Recognize Your Most Fertile Days
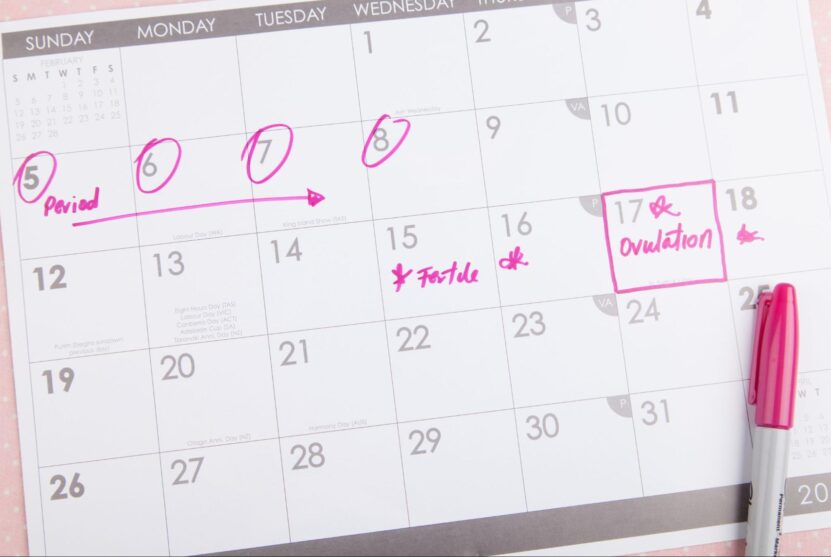
Ovulation is a key event in the menstrual cycle, marking the release of a mature egg from the ovary into the fallopian tube, where fertilization can occur. Recognizing the signs of ovulation is crucial for those trying to conceive and those monitoring their reproductive health. By understanding ovulation symptoms, tracking ovulation, and using tools like ovulation predictor kits, you can predict ovulation with greater accuracy. This guide will help you identify ovulation signs, learn about ovulation patterns, and understand how to track ovulation effectively.
Understanding Ovulation and the Menstrual Cycle
The menstrual cycle typically lasts between 21 to 35 days and consists of four phases:
- Menstrual Phase – The shedding of the uterine lining, marking the start of a new cycle.
- Follicular Phase – Estrogen levels rise, stimulating follicle growth in the ovaries.
- Ovulation Phase – A surge in luteinizing hormone (LH) triggers ovulation, when the mature egg is released.
- Luteal Phase – Progesterone prepares the uterus for potential implantation of a fertilized egg.
Ovulation typically occurs around day 14 in a 28-day cycle, but this varies among individuals. Identifying ovulation patterns through consistent tracking can help pinpoint your fertile window—the days when conception is most likely.
Common Signs of Ovulation
Recognizing ovulation symptoms can help you track ovulation more effectively. Here are some of the most common ovulation signs:
1. Basal Body Temperature (BBT) Changes
Basal body temperature (BBT) is your lowest body temperature at rest. Before ovulation, BBT is relatively consistent. After ovulation occurs, progesterone causes a slight rise (0.5–1.0°F). By charting your BBT over several months, you can identify when ovulation typically happens.
2. Cervical Mucus Consistency and Changes
Cervical mucus consistency changes throughout the menstrual cycle. As ovulation approaches, it becomes clear, stretchy, and similar to egg whites, creating a sperm-friendly environment. Monitoring cervical mucus changes can help predict ovulation.
3. Ovulation Pain (Mittelschmerz)
Some women experience ovulation pain, known as mittelschmerz, as a mild ache or cramping on one side of the lower abdomen. This pain usually lasts a few hours to a couple of days and indicates that ovulation has occurred.
4. Increased Libido and Energy Levels
Many women report heightened sexual desire around their fertile days due to hormonal shifts. A surge in estrogen levels may also boost mood and energy levels.
5. Breast Tenderness
Breast tenderness or sensitivity is another common ovulation symptom. Hormonal changes during the ovulation phase can cause temporary discomfort.
6. Light Spotting or Ovulation Discharge
Some women experience light spotting or ovulation discharge due to the rupture of the follicle releasing the egg. This is usually harmless but should be monitored.
7. Heightened Senses
Some women report an increased sense of smell, taste, or vision around ovulation due to hormonal fluctuations.
How to Track Ovulation Effectively
Tracking ovulation is essential for understanding your reproductive health. Here are several methods to help predict ovulation:
1. Using an Ovulation Predictor Kit (OPK)
Ovulation predictor kits (OPKs) identify the rise in luteinizing hormone (LH) that occurs before ovulation. A positive test suggests ovulation will likely occur within 12–36 hours. This is one of the most reliable ways to track ovulation.
2. Charting Basal Body Temperature (BBT)
By measuring your BBT every morning before getting out of bed, you can identify temperature patterns indicating ovulation has occurred. While this method does not predict ovulation in advance, it helps track ovulation retrospectively.
3. Monitoring Cervical Mucus
Observing changes in cervical mucus consistency can help you identify when you are most fertile. Egg white-like mucus signals that you are in your fertile window.
4. Tracking Menstrual Cycle Length and Ovulation Date
Using a menstrual cycle tracker or ovulation calculator can help predict ovulation based on previous cycles. Apps designed for fertility tracking can provide insights into ovulation patterns.
5. Paying Attention to Ovulation Symptoms
Keeping a journal of symptoms such as ovulation pain, breast tenderness, and libido changes can help identify ovulation patterns.
Factors That Can Affect Ovulation
1. Polycystic Ovary Syndrome (PCOS)
PCOS can cause irregular ovulation or anovulation (absence of ovulation). Women with PCOS often have irregular menstrual cycles, making ovulation more difficult to predict.
2. Stress and Lifestyle Factors
High stress levels, excessive exercise, and sudden weight changes can disrupt hormone levels, leading to irregular ovulation.
3. Premature Ovarian Failure
Premature ovarian failure, also known as primary ovarian insufficiency, involves the loss of normal ovarian function before age 40, resulting in irregular ovulation.
When to See a Doctor
If you experience irregular ovulation, have concerns about your menstrual cycle, or have been trying to conceive without success, consult a healthcare provider. They can evaluate your hormone levels, check for conditions like PCOS, and recommend fertility treatments if necessary.
Final Thoughts
Tracking ovulation is crucial for understanding your reproductive health, whether you’re trying to conceive or monitoring fertility for birth control. By recognizing ovulation symptoms, monitoring cervical mucus consistency, and using tools like ovulation predictor kits, you can better predict ovulation and identify your fertile days. If you have concerns about your ovulation patterns or experience irregular ovulation, seek medical advice to explore potential solutions.


